Short upfront: if you or someone you love has been diagnosed with cancer, the best outcomes come from evidence-based cancer care (surgery, radiation, systemic therapy when indicated) plus safe, well-chosen complementary measures that improve symptoms, quality of life, and sometimes outcomes. Choosing only “natural” or alternative therapies in place of conventional cancer treatment has been linked to substantially worse survival. (Cancer.gov)
Below I give a detailed, practical, and referenced guide to natural and complementary approaches you might consider, what the evidence does — and does not — show, safety cautions, and how to discuss these options with your oncology team.
1) An important safety principle (do this first)
Never replace standard cancer treatments with unproven natural therapies. Large studies show that patients who choose alternative therapies instead of conventional cancer treatment have a much higher risk of dying. Complementary treatments are best used alongside standard care to manage symptoms and improve well-being. Discuss everything you plan to take or do with your oncologist (drug interactions and timing with chemo/radiation matter). (Cancer.gov)
2) Interventions with the strongest evidence for benefit (and how they help)
Exercise and structured physical activity

What it does: improves fatigue, physical functioning, mood, cardiorespiratory fitness — and recent high-quality trials show exercise after treatment can reduce recurrence and death for some cancers (e.g., colon cancer), making it a powerful adjuvant measure. Aim for individualized, supervised programs if you’re recovering from surgery or on active treatment. (The Guardian)
Practical tips:
- Start with what you can tolerate (walking, light resistance training).
- Seek oncology-rehabilitation or physiotherapy programs when available.
- If on active treatment, get clearance from your oncologist and avoid heavy lifting if you have low blood counts or bone metastases.
Nutrition and body weight

What it does: maintaining a healthy weight, a mostly plant-based diet, and avoiding excess alcohol are associated with better outcomes in many cancers (and lower recurrence risk in some tumour types). Good nutrition also reduces treatment side effects and supports recovery.
Practical tips:
- Focus on whole foods: vegetables, fruits, legumes, whole grains, healthy fats, and lean proteins.
- Avoid crash diets during active treatment; instead, aim for steady, adequate nutrition and protein to preserve muscle.
- Work with an oncology dietitian for individualized plan — especially if weight loss, swallowing problems, or GI side effects are present.
Vitamin D (monitor and correct deficiency)
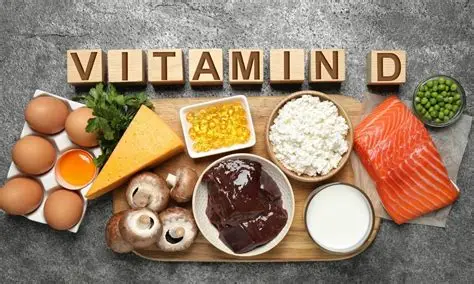
What it does: observational data link higher vitamin D levels to better outcomes in some cancers, and randomized trials show modest reductions in cancer mortality with supplementation in some analyses — but evidence is mixed and dosing should be individualized. Have serum 25-OH vitamin D checked and correct deficiency under medical supervision. (PubMed Central)
Practical tip: Don’t self-prescribe mega-doses. Work with your clinician to pick a safe dose and monitor blood levels.
Symptom relief and quality-of-life interventions with good evidence
- Acupuncture: helpful for chemotherapy-induced nausea/vomiting, some types of pain, hot flashes, and fatigue in cancer patients. It’s frequently used as an adjunct to reduce medication needs and improve comfort. (Use licensed practitioners experienced with oncology patients.) (Cancer.gov)
- Mind-body therapies (CBT, mindfulness, meditation, tai chi, yoga): reduce anxiety, depression, and cancer-related fatigue; improve sleep and coping. Evidence supports their use as adjunctive therapies. (NCCIH)
3) Popular “natural” agents — what the evidence and safety data say
Important: “Natural” ≠ harmless. Many herbs and supplements interact with chemo, immunotherapy, or increase bleeding/infection risk.
Curcumin (turmeric)

- Evidence: laboratory and early clinical trials show anti-inflammatory and anticancer effects; human clinical data are mixed and mostly early-phase. The NCI PDQ review notes ongoing trials and some safety signals but not definitive proof that curcumin cures cancer. Can reduce some liver enzymes and has been studied as an adjunct. (Cancer.gov)
- Cautions: poor oral absorption (formulation matters); can interact with anticoagulants and some drugs; high doses may cause GI upset or affect liver tests.
Green tea (EGCG)
- Evidence: observational and some trial data suggest possible protective associations for certain cancers; meta-analyses show mixed results and dose–response is unclear. High-dose extracts can have liver toxicity in rare cases. (PubMed)
Medicinal mushrooms (e.g., Turkey tail, Reishi)

- Evidence: some randomized and observational studies (especially from Asia) suggest mushrooms may improve immune responses and possibly survival as adjuncts; data vary by mushroom species and study quality. They are used as adjunctive therapy in parts of Asia. (Cancer.gov)
- Cautions: product quality varies; possible immune modulation — discuss with oncologist, especially if you’re on immunotherapy.
Mistletoe (viscum album)

- Evidence: mixed. Some controlled trials and systematic reviews report improved quality of life and symptom control; research quality varies and it is not widely used or approved in many countries. Ongoing studies are small and heterogeneous. (NCBI)
- Cautions: injection therapies should only be administered by qualified providers; possible injection-site reactions and systemic effects.
Cannabinoids (medical cannabis)
- Evidence: effective for chemotherapy-related nausea when traditional antiemetics fail, and for cancer-related pain and appetite stimulation in some patients; evidence for anticancer effects in humans is not established. Discuss legal/medical status and potential interactions (sedation, cognition, immune effects).
Supplements to be cautious about
- Antioxidant supplements (high-dose vitamin E, beta-carotene): have sometimes shown harm or increased risk in certain cancer populations (for example, smokers). Avoid indiscriminate high-dose antioxidant therapy during active treatment unless specifically advised by your oncology team.
- Herbs that affect blood clotting or liver enzymes (e.g., ginkgo, garlic in high doses, St. John’s wort) can interact with chemotherapy or targeted agents.
4) How to evaluate a natural therapy (a practical checklist)
- Is there randomized clinical trial evidence? Prioritize interventions with RCT data.
- Mechanism plausibility + human data: preclinical benefit is encouraging but not proof.
- Safety / interactions: check with pharmacist or oncologist (especially for anticoagulants, enzyme inducers/inhibitors, immunotherapies).
- Product quality: choose reputable manufacturers with third-party testing (USP, NSF, independent lab certificates).
- Cost and access: avoid expensive, unproven “cures.”
- Regulation status: is it legal and used in clinical practice in your country?
5) Practical, step-by-step plan you can use (immediately)
- Prioritize evidence-based cancer treatment recommended by your oncology team. (If you are unsure or doubt recommendations, seek a second opinion.) (Cancer.gov)
- Ask for baseline tests: vitamin D level, nutritional assessment, and review of current medications/supplements for interactions.
- Start safe complementary measures: supervised exercise program, referral to oncology dietitian, mind-body therapy (CBT/mindfulness), and acupuncture for symptomatic relief where appropriate. (The Guardian)
- If considering supplements or herbs (curcumin, mushrooms, vitamin D, cannabis, etc.), bring the specific product label to your oncologist or oncology pharmacist and discuss timing relative to chemo/immunotherapy.
- Document everything you take, and have regular follow-ups to monitor labs, side effects, and interactions.
6) When “natural” treatments can be dangerous
- Using alternative treatments instead of recommended, curative therapies for early-stage, potentially curable cancers. Evidence shows higher mortality when patients delay/decline conventional therapy. (Cancer.gov)
- Unregulated intravenous “natural” infusions (high risk of infection, contamination, or interactions).
- High-dose supplements without monitoring (e.g., fat-soluble vitamins) or herbs that interfere with therapy.
7) Questions to ask your oncologist or integrative medicine specialist
- Could this supplement interact with my chemo/immunotherapy/radiation?
- Is there evidence it helps my cancer type or symptoms?
- What dose and duration are reasonable and safe?
- Should we monitor labs (liver, kidneys, blood counts) while I take it?
- Can you refer me to a certified oncology nutritionist, physiotherapist, or integrative medicine clinic?
8) Reliable resources and where to read more
- National Cancer Institute (NCI) — complementary and alternative medicine pages (detailed PDQ reviews for curcumin, mushrooms, acupuncture). (Cancer.gov)
- National Center for Complementary and Integrative Health (NCCIH) — evidence summaries for mind-body and acupuncture. (NCCIH)
- Cochrane Library — systematic reviews of many complementary therapies. (cam.cochrane.org)
9) Final summary (bottom line)
- Do not abandon proven cancer treatments in favor of natural remedies. Patients who do so have worse survival. (Cancer.gov)
- Do use evidence-based complementary practices to improve symptoms, quality of life, and possibly outcomes: supervised exercise, nutrition optimization, vitamin D correction (if deficient), acupuncture for specific symptoms, and mind-body therapies. (The Guardian)


Your point of view caught my eye and was very interesting. Thanks. I have a question for you.